Abstract
Background
Treatment of multiple myeloma (MM) has changed significantly in recent years with the availability of novel agents including monoclonal antibodies (mAbs), proteasome inhibitors (PIs) and immunomodulatory drugs (IMiDs) such as lenalidomide. Despite lenalidomide becoming a standard of care across all lines of myeloma therapy, the population of MM patients refractory to lenalidomide and their real-world clinical management has been poorly studied so far, especially outside the reality of interventional clinical trials (Moreau et. al. Blood Cancer J. 2019).
With these considerations in mind, we have performed a retrospective study using two databases to better understand treatment patterns and outcomes of MM patients who were treated with lenalidomide and subsequently became refractory to it. This builds on work previously conducted at other data sources (Willenbacher et. al. EHA Library 2020).
Aims
The objective of this study was to describe the treatment patterns and outcomes of MM patients exposed to lenalidomide, with a focus on refractory patients, as defined by IMWG (International Myeloma Working Group) consensus, in a real-world clinical setting.
Methods
The study utilised databases from two participating members of the IQVIA MM real world evidence network: University Hospital Frankfurt (Frankfurt) (Germany) and Portuguese Oncology Institute of Porto (IPO-Porto) (Portugal). Since the native format of databases from participating sites differs, key concepts were harmonised based on pre-agreed definitions. The study population included patients with an initial diagnosis of MM between 01/01/2012 and 31/12/2018 based on the IMWG criteria, were 18 years old or older at the time of diagnosis and received two or more cycles of lenalidomide treatment, alone or in combination, at any dose, excluding patients who only received lenalidomide as maintenance therapy. Patients were defined as refractory to lenalidomide treatment if they progressed on treatment or within 60 days following the end of lenalidomide treatment (excluding maintenance setting).
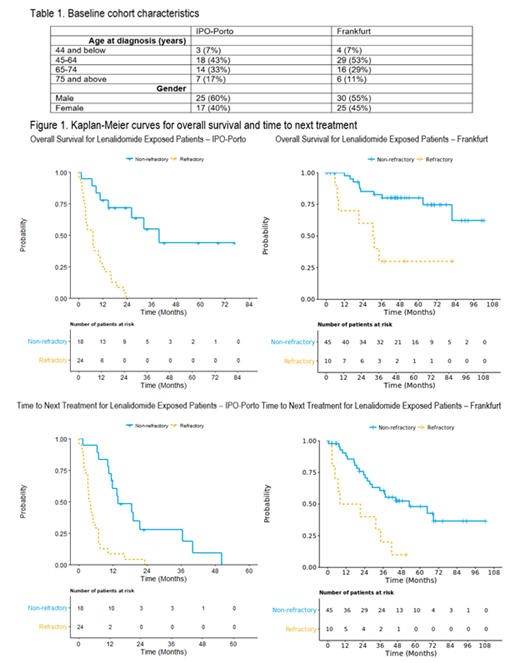
Kaplan-Meier curves were produced to evaluate the time to next treatment (TTNT) and overall survival (OS) for lenalidomide exposed and lenalidomide refractory patients. TTNT was defined as the time between the start date of the line of lenalidomide therapy and the start date of the next line of therapy (LoT) or death due to any cause. OS was defined as the time between the start date of the line of lenalidomide therapy and death due to any cause.
Results
The cohort included 55 and 42 MM lenalidomide-exposed patients from Germany and Portugal respectively. In Germany, 80% were initially exposed to the lenalidomide in LoT 1, whilst in Portugal 71% received initial lenalidomide treatment in LoT 3.
In Portugal, following lenalidomide refractoriness, the majority (78%) of patients received chemotherapy and steroids only whilst in Germany a range of treatment types was observed (mAb-based 33%; PI-based 11%; PI/IMiD combo 11%; mAb/IMiD combo 11%; chemotherapy and steroids only 11%; other 22%).
The median OS in months for lenalidomide-exposed refractory patients was 7 in Portugal and 31 in Germany; the median OS for non-refractory patients was 40 in Portugal and was not reached in Germany.
The median TTNT in months for lenalidomide-exposed refractory patients was 4 in Portugal and 15 in Germany; the median TTNT for non-refractory patients was 14 in Portugal and 53 in Germany.
Conclusion
The analysis of real-world data across two countries, showed heterogeneity in lenalidomide treatment patterns, with first exposure typically occurring in LoT 1 or 3. This has led to differences in the calculated TTNT and OS, and as such the results between the two countries cannot be directly compared. The OS from diagnosis for this cohort is being assessed and will provide an insight on the impact of different treatment pathways.
Patients who became refractory to lenalidomide moved on to their next treatment much quicker after exposure vs patients who were not refractory to lenalidomide; similarly, patients who became refractory to lenalidomide had shorter OS than patients who were not refractory.
Patients typically became refractory early in their treatment journey, indicating a growing population with unmet medical needs.
Metzler: GSK: Consultancy; Takeda: Consultancy; Janssen: Consultancy; AstraZeneca: Consultancy; Amgen: Consultancy; BMS: Consultancy; Sanofi: Consultancy; Pfizer: Consultancy.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal